We’re hiring a postdoc in environmental AMR monitoring
As part of the SEARCHER program, we are now hiring a two-year postdoc to work with innovative approaches to antibiotic resistance monitoring. You can read more about the position here and at Chalmers’ job portal, but in short we are after a wet-lab postdoc who are willing to do field work and laboratory studies to identify novel antibiotic resistance genes.
Please do not send me your CV and application letter via e-mail, but apply through the Chalmers application portal. Sending your CV to me will not increase your changes. Only contact me about this position if you have actual, relevant questions about the position (as I will otherwise get lots of unwanted e-mails…) Those questions, I am happy to answer!
Published papers: Environmental monitoring of antibiotic resistance
In just a few days, Environment International has published two papers coming out from the EMBARK consortium which are somewhat connected to each other.
The first (or technically the second, but the other order makes more sense when explaining this…) is the first paper involving most of the people who have been working in the EMBARK consortium for an extended period of time. It’s an overview paper titled “Towards monitoring of antimicrobial resistance in the environment: For what reasons, how to implement Itit, and what are the data needs?” (1) and I think the title describes the topic pretty well. Basically, we go through why it would be interesting to monitor for antibiotic resistance in the environments, how that could be implemented and what we would need to know to get there.
The very condensed story is that if one is considering implementing monitoring for environmental resistance, these are a few things that should be considered:
- The purpose of monitoring: What is the motivation? What should be achieved? What type of risk should be assessed? What type of action would monitoring enable?
- Choice of methods: Which methods are economically feasible? Which methods would deliver results within a useful timeframe for taking appropriate actions?
- Targeted environments: In what type of environment would monitoring for a given purpose be worthwhile?
- Intended users: Who would be able to use, implement and act upon this strategy?
- Integration potential: How does this monitoring integrate with other monitoring efforts? How can the resulting data be communicated?
We then dive into the knowledge gaps we are currently facing, and particularly highlight the following areas:
- Establish how different existing methods for monitoring resistance compare to each other
- Extend pathogen-centric databases for resistance genes with latent resistance genes (2)
- Determine the locations and type of environments relevant for resistance monitoring
To reduce costs, utilizing already existing environmental monitoring should be prioritized, as should locations integrated into operating or planned surveillance programs. More efforts should also be made to identify additional pathways for resistance transmission through the environment. - Study the environment as a source and transmission route for antibiotic resistance
Stratify risks associated with resistance genes found in the environment. Define typical levels of antibiotic resistance in different environments (3), and define how these levels change over time. - Identify settings where the relationship between fecal bacteria and antibiotic resistance is absent
Usually, these levels follow each other, but the environments where they don’t are important as they deviate from the expected baseline of resistance. This knowledge can aid in identifying situations in which it would be helpful to investigate a microbial community for resistance to specific antibiotics. - Identify the origins for more antibiotic resistance genes (4)
This knowledge will be instrumental in preventing the emergence of new forms of resistance in pathogens in the future.
An important outcome of this paper is that we realise that we are still not at a level of understanding where routine monitoring for resistance in the environment can be easily justified or implemented. Still, there is a need for monitoring data in natural environments to even get started, and therefore we support the implementation of national, regional and global of initiatives without having all the scientific answers. The lack of comprehensive understanding should not be an obstacle to starting environmental monitoring for AMR, nor for action against environmental development and spread of AMR.
The second paper is very much related to the first, in that it actually tries to address one of these knowledge gaps: the need for normal background levels of antibiotic resistance in different environments. In this paper, Anna Abramova did an herculean effort collecting (we hope) all qPCR data on antibiotic resistance gene abundances in the environment for the past two decades. All in all, she collected data for more than 1500 samples across 150 studies and integrated these into an analys of what we could consider normal levels of resistance in different environments.
For an ‘average’ resistance gene, we found that the normal relative abundance range was form 10-5 to 10-3 copies per bacterial 16S rRNA, or that around one in 1,000 bacteria would carry a given resistance gene. This level varied quite a bit between different resistance genes, however, but not so much between environmental types (except for in human and animal feces, where some resistance genes were clearly more abundant, most prominently tetracycline resistance genes). What was more striking was that there was a clear difference between environments impacted or likely impacted by human activities, as opposed to more pristine environments with little to none human impact. Some resistance genes, such as tetA, tetG, blaTEM and blaCTX-M, showed very marked differences between these impacted and non-impacted environments, making them great markers of human-activity-associated resistance.
Our final recommendations with regards to monitoring include:
- Include the intI1, sul1, blaTEM, blaCTX-M and qnrS genes in environmental monitoring, along with a selection of tetracycline resistance genes, including either tetA or tetG.
- Other potential target genes could be sul3, vanA, tetH, aadA2, floR, ereA and mexF, which are abundant in some environments, but are not often included in qPCR studies of environmental AMR
- If a gene deviates from the expected 10-5 to 10-3 interval, this warrants further investigation of the causes.
- Maximum acceptable levels need to be determined not only taking relative abundances of genes into account, but also risks to human health as well as the numbers of bacteria in a given volume of sample into account (5,6) and transmission routes to humans (7)
- The different standards of reporting DNA abundances constituted a complicating factor for this study. Both abundances of resistance genes relative to the 16S rRNA gene and to the sample volume or weight should be reported.
- The absence of clear trends of increases or decreases in resistance gene abundances over time indicates a need for more systematic time series data in a variety of environments.
Our results also highlighted the scarcity of resistance gene data from parts of the world, particularly from Africa and South America, and underscores the need for a concerted effort to quantify typical background levels of resistance in the environment more broadly to enable efficient environmental surveillance schemes akin to those that exist in clinical and veterinary settings.
I encourage anyone with an interesting these topics to at least skim the full papers [Monitoring overview paper here, Normal qPCR resistance abundances here]. These will be great resources and I am very proud of them both. I would really like to thank the entire EMBARK team and our collaborators in CORNELIA, WastPAN and in other organisations. I would also like to thank Anna for her hard work on collecting and analysing the qPCR data for around two years. It has been a long ride, and I think we are both happy, proud and a bit relieved to finally see this paper published!
References
- Bengtsson-Palme J, Abramova A, Berendonk TU, Coelho LP, Forslund SK, Gschwind R, Heikinheimo A, Jarquin-Diaz VH, Khan AA, Klümper U, Löber U, Nekoro M, Osińska AD, Ugarcina Perovic S, Pitkänen T, Rødland EK, Ruppé E, Wasteson Y, Wester AL, Zahra R: Towards monitoring of antimicrobial resistance in the environment: For what reasons, how to implement it, and what are the data needs? Environment International, 108089 (2023). doi: 10.1016/j.envint.2023.108089
- Inda-Díaz JS, Lund D, Parras-Moltó M, Johnning A, Bengtsson-Palme J, Kristiansson E: Latent antibiotic resistance genes are abundant, diverse, and mobile in human, animal, and environmental microbiomes. Microbiome, 11, 44 (2023). doi: 10.1186/s40168-023-01479-0
- Abramova A, Berendonk TU, Bengtsson-Palme J: A global baseline for qPCR-determined antimicrobial resistance gene prevalence across environments. Environment International, 178, 108084 (2023). doi: 10.1016/j.envint.2023.108084
- Ebmeyer S, Kristiansson E, Larsson DGJ: A framework for identifying the recent origins of mobile antibiotic resistance genes. Communications Biology, 4 (2021). doi:10.1038/s42003-020-01545-5
- Larsson DGJ, Andremont A, Bengtsson-Palme J, Brandt KK, de Roda Husman AM, Fagerstedt P, Fick J, Flach C-F, Gaze WH, Kuroda M, Kvint K, Laxminarayan R, Manaia CM, Nielsen KM, Ploy M-C, Segovia C, Simonet P, Smalla K, Snape J, Topp E, van Hengel A, Verner-Jeffreys DW, Virta MPJ, Wellington EM, Wernersson A-S: Critical knowledge gaps and research needs related to the environmental dimensions of antibiotic resistance. Environment International, 117, 132–138 (2018). doi: 10.1016/j.envint.2018.04.041
- Pruden A, Larsson DGJ, Amézquita A, Collignon P, Brandt KK, Graham DW, et al. Management options for reducing the release of antibiotics and antibiotic resistance genes to the environment. Environmental Health Perspectives, 121, 878–885 (2013). doi:10.1289/ehp.1206446
- Bengtsson-Palme J, Kristiansson E, Larsson DGJ: Environmental factors influencing the development and spread of antibiotic resistance. FEMS Microbiology Reviews, 42, 1, 68–80 (2018). doi: 10.1093/femsre/fux053
Published paper: Knowledge gaps for environmental antibiotic resistance
The outcomes from a workshop arranged by JPIAMR, the Swedish Research Council (VR) and CARe were just published as a short review paper in Environment International. In the paper, which was mostly moved forward by Prof. Joakim Larsson at CARe, we describe four major areas of knowledge gaps in the realm of environmental antibiotic resistance (1). We then highlight several important sub-questions within these areas. The broad areas we define are:
- What are the relative contributions of different sources of antibiotics and antibiotic resistant bacteria into the environment?
- What is the role of the environment as affected by anthropogenic inputs (e.g. pollution and other activities) on the evolution (mobilization, selection, transfer, persistence etc.) of antibiotic resistance?
- How significant is the exposure of humans to antibiotic resistant bacteria via different environmental routes, and what is the impact on human health?
- What technological, social, economic and behavioral interventions are effective to mitigate the emergence and spread of antibiotic resistance via the environment?
Although much has been written on the topic before (e.g. 2-12), I think it is unique that we collect and explicitly point out areas in which we are lacking important knowledge to build accurate risk models and devise appropriate intervention strategies. The workshop was held in Gothenburg on the 27–28th of September 2017. The workshop leaders Joakim Larsson, Ana-Maria de Roda Husman and Ramanan Laxminarayan were each responsible for moderating a breakout group, and every breakout group was tasked to deal with knowledge gaps related to either evolution, transmission or interventions. The reports of the breakout groups were then discussed among all participants to clarify and structure the areas where more research is needed, which boiled down to the four overarching critical knowledge gaps described in the paper (1).
This is a short paper, and I think everyone with an interest in environmental antibiotic resistance should read it and reflect over its content (because, we may of course have overlooked some important aspect). You can find the paper here.
References
- Larsson DGJ, Andremont A, Bengtsson-Palme J, Brandt KK, de Roda Husman AM, Fagerstedt P, Fick J, Flach C-F, Gaze WH, Kuroda M, Kvint K, Laxminarayan R, Manaia CM, Nielsen KM, Ploy M-C, Segovia C, Simonet P, Smalla K, Snape J, Topp E, van Hengel A, Verner-Jeffreys DW, Virta MPJ, Wellington EM, Wernersson A-S: Critical knowledge gaps and research needs related to the environmental dimensions of antibiotic resistance. Environment International, 117, 132–138 (2018). doi: 10.1016/j.envint.2018.04.041
- Bengtsson-Palme J, Kristiansson E, Larsson DGJ: Environmental factors influencing the development and spread of antibiotic resistance. FEMS Microbiology Reviews, 42, 1, 68–80 (2018). doi: 10.1093/femsre/fux053
- Martinez JL, Coque TM, Baquero F: What is a resistance gene? Ranking risk in resistomes. Nature Reviews Microbiology 2015, 13:116–123. doi:10.1038/nrmicro3399
- Bengtsson-Palme J, Larsson DGJ: Antibiotic resistance genes in the environment: prioritizing risks. Nature Reviews Microbiology, 13, 369 (2015). doi: 10.1038/nrmicro3399-c1
- Ashbolt NJ, Amézquita A, Backhaus T, Borriello P, Brandt KK, Collignon P, et al.: Human Health Risk Assessment (HHRA) for Environmental Development and Transfer of Antibiotic Resistance. Environmental Health Perspectives, 121, 993–1001 (2013)
- Pruden A, Larsson DGJ, Amézquita A, Collignon P, Brandt KK, Graham DW, et al.: Management options for reducing the release of antibiotics and antibiotic resistance genes to the environment. Environmental Health Perspectives, 121, 878–85 (2013).
- Gillings MR: Evolutionary consequences of antibiotic use for the resistome, mobilome and microbial pangenome. Frontiers in Microbiology, 4, 4 (2013).
- Baquero F, Alvarez-Ortega C, Martinez JL: Ecology and evolution of antibiotic resistance. Environmental Microbiology Reports, 1, 469–476 (2009).
- Baquero F, Tedim AP, Coque TM: Antibiotic resistance shaping multi-level population biology of bacteria. Frontiers in Microbiology, 4, 15 (2013).
- Berendonk TU, Manaia CM, Merlin C et al.: Tackling antibiotic resistance: the environmental framework. Nature Reviews Microbiology, 13, 310–317 (2015).
- Hiltunen T, Virta M, Laine A-L: Antibiotic resistance in the wild: an eco-evolutionary perspective. Philosophical Transactions of the Royal Society B: Biological Sciences, 372 (2017) doi: 10.1098/rstb.2016.0039.
- Martinez JL: Bottlenecks in the transferability of antibiotic resistance from natural ecosystems to human bacterial pathogens. Frontiers in Microbiology, 2, 265 (2011).
Published paper: Environmental factors leading to resistance
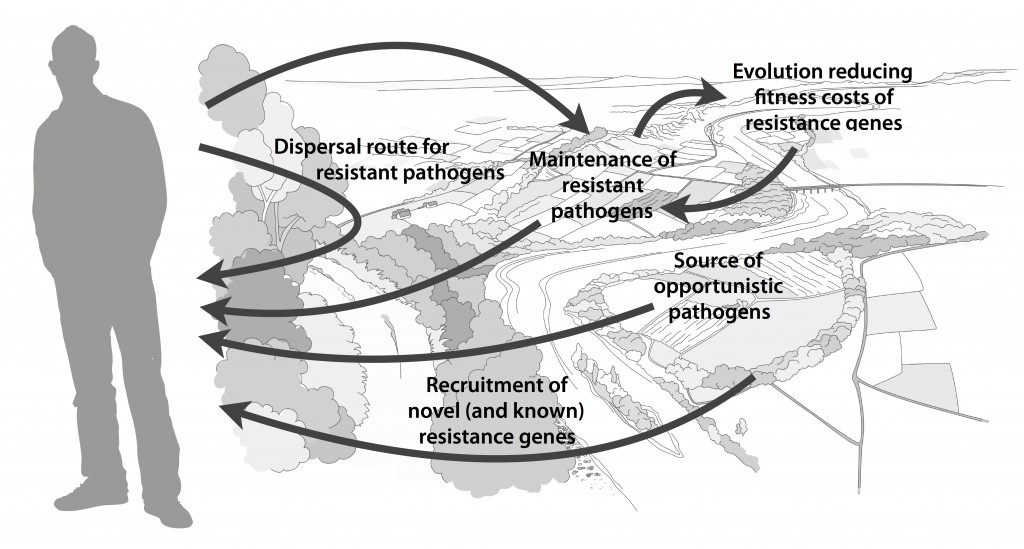
Myself, Joakim Larsson and Erik Kristiansson have written a review on the environmental factors that influence development and spread of antibiotic resistance, which was published today in FEMS Microbiology Reviews. The review (1) builds on thoughts developed in the latter parts of my PhD thesis (2), and seeks to provide a synthesis knowledge gained from different subfields towards the current understanding of evolutionary and ecological processes leading to clinical appearance of resistance genes, as well as the important environmental dispersal barriers preventing spread of resistant pathogens.
We postulate that emergence of novel resistance factors and mobilization of resistance genes are likely to occur continuously in the environment. However, the great majority of such genetic events are unlikely to lead to establishment of novel resistance factors in bacterial populations, unless there is a selection pressure for maintaining them or their fitness costs are negligible. To enable measures to prevent resistance development in the environment, it is therefore critical to investigate under what conditions and to what extent environmental selection for resistance takes place. Selection for resistance is likely less important for the dissemination of resistant bacteria, but will ultimately depend on how well the species or strain in question thrives in the external environment. Metacommunity theory (3,4) suggests that dispersal ability is central to this process, and therefore opportunistic pathogens with their main habitat in the environment may play an important role in the exchange of resistance factors between humans and the environment. Understanding the dispersal barriers hindering this exchange is not only key to evaluate risks, but also to prevent resistant pathogens, as well as novel resistance genes, from reaching humans.
Towards the end of the paper, we suggest certain environments that seem to be more important from a risk management perspective. We also discuss additional problems linked to the development of antibiotic resistance, such as increased evolvability of bacterial genomes (5) and which other types of genes that may be mobilized in the future, should the development continue (1,6). In this review, we also further develop thoughts on the relative risks of re-recruiting and spreading well-known resistance factors already circulating in pathogens, versus recruitment of completely novel resistance genes from environmental bacteria (7). While the latter case is likely to be very rare, and thus almost impossible to quantify the risks for, the consequences of such (potentially one-time) events can be dire.
I personally think that this is one of the best though-through pieces I have ever written, and since it is open access and (in my biased opinion) written in a fairly accessible way, I recommend everyone to read it. It builds on the ecological theories for resistance ecology developed by, among others, Fernando Baquero and José Martinez (8-13). Over the last year, it has been stressed several times at meetings (e.g. at the EDAR conferences in August) that there is a need to develop an ecological framework for antibiotic resistance genes. I think this paper could be one of the foundational pillars on such an endeavor and look forward to see how it will fit into the growing literature on the subject!
References
- Bengtsson-Palme J, Kristiansson E, Larsson DGJ: Environmental factors influencing the development and spread of antibiotic resistance. FEMS Microbiology Reviews, accepted manuscript (2017). doi: 10.1093/femsre/fux053
- Bengtsson-Palme J: Antibiotic resistance in the environment: a contribution from metagenomic studies. Doctoral thesis (medicine), Department of Infectious Diseases, Institute of Biomedicine, Sahlgrenska Academy, University of Gothenburg, 2016. [Link]
- Bengtsson J: Applied (meta)community ecology: diversity and ecosystem services at the intersection of local and regional processes. In: Verhoef HA, Morin PJ (eds.). Community Ecology: Processes, Models, and Applications. Oxford: Oxford University Press, 115–130 (2009).
- Leibold M, Norberg J: Biodiversity in metacommunities: Plankton as complex adaptive systems? Limnology and Oceanography, 1278–1289 (2004).
- Gillings MR, Stokes HW: Are humans increasing bacterial evolvability? Trends in Ecology and Evolution, 27, 346–352 (2012).
- Gillings MR: Evolutionary consequences of antibiotic use for the resistome, mobilome and microbial pangenome. Frontiers in Microbiology, 4, 4 (2013).
- Bengtsson-Palme J, Larsson DGJ: Antibiotic resistance genes in the environment: prioritizing risks. Nature Reviews Microbiology, 13, 369 (2015). doi: 10.1038/nrmicro3399-c1
- Baquero F, Alvarez-Ortega C, Martinez JL: Ecology and evolution of antibiotic resistance. Environmental Microbiology Reports, 1, 469–476 (2009).
- Baquero F, Tedim AP, Coque TM: Antibiotic resistance shaping multi-level population biology of bacteria. Frontiers in Microbiology, 4, 15 (2013).
- Berendonk TU, Manaia CM, Merlin C et al.: Tackling antibiotic resistance: the environmental framework. Nature Reviews Microbiology, 13, 310–317 (2015).
- Hiltunen T, Virta M, Laine A-L: Antibiotic resistance in the wild: an eco-evolutionary perspective. Philosophical Transactions of the Royal Society B: Biological Sciences, 372 (2017) doi: 10.1098/rstb.2016.0039.
- Martinez JL: Bottlenecks in the transferability of antibiotic resistance from natural ecosystems to human bacterial pathogens. Frontiers in Microbiology, 2, 265 (2011).
- Salyers AA, Amábile-Cuevas CF: Why are antibiotic resistance genes so resistant to elimination? Antimicrobial Agents and Chemotherapy, 41, 2321–2325 (1997).
Published paper: The global resistome
Late yesterday, Microbiome put online our most recent work, covering the resistomes to antibiotics, biocides and metals across a vast range of environments. In the paper (1), we perform the largest characterization of resistance genes, mobile genetic elements (MGEs) and bacterial taxonomic compositions to date, covering 864 different metagenomes from humans (350), animals (145) and external environments such as soil, water, sewage, and air (369 in total). All the investigated metagenomes were sequenced to at least 10 million reads each, using Illumina technology, making the results more comparable across environments than in previous studies (2-4).
We found that the environment types had clear differences both in terms of resistance profiles and bacterial community composition. Humans and animals hosted microbial communities with limited taxonomic diversity as well as low abundance and diversity of biocide/metal resistance genes and MGEs. On the contrary, the abundance of ARGs was relatively high in humans and animals. External environments, on the other hand, showed high taxonomic diversity and high diversity of biocide/metal resistance genes and MGEs. Water, sediment and soil generally carried low relative abundance and few varieties of known ARGs, whereas wastewater and sludge were on par with the human gut. The environments with the largest relative abundance and diversity of ARGs, including genes encoding resistance to last resort antibiotics, were those subjected to industrial antibiotic pollution and air samples from a Beijing smog event.
A paper investigating this vast amount of data is of course hard to describe in a blog post, so I strongly suggest the interested reader to head over to Microbiome’s page and read the full paper (1). However, here’s a ver short summary of the findings:
- The median relative abundance of ARGs across all environments was 0.035 copies per bacterial 16S rRNA
- Antibiotic-polluted environments have (by far) the highest abundances of ARGs
- Urban air samples carried high abundance and diversity of ARGs
- Human microbiota has high abundance and diversity of known ARGs, but low taxonomic diversity compared to the external environment
- The human and animal resistomes are dominated by tetracycline resistance genes
- Over half of the ARGs were only detected in external environments, while 20.5 % were found in human, animal and at least one of the external environments
- Biocide and metal resistance genes are more common in external environments than in the human microbiota
- Human microbiota carries low abundance and richness of MGEs compared to most external environments
Importantly, less than 1.5 % of all detected ARGs were found exclusively in the human microbiome. At the same time, 57.5 % of the known ARGs were only detected in metagenomes from environmental samples, despite that the majority of the investigated ARGs were initially encountered in pathogens. Still, our analysis suggests that most of these genes are relatively rare in the human microbiota. Environmental samples generally contained a wider distribution of resistance genes to a more diverse set of antibiotics classes. For example, the relative abundance of beta-lactam resistance genes was much larger in external environments than in human and animal microbiomes. This suggests that the external environment harbours many more varieties of resistance genes than the ones currently known from the clinic. Indeed, functional metagenomics has resulted in the discovery of many novel ARGs in external environments (e.g. 5). This all fits well with an overall much higher taxonomic diversity of environmental microbial communities. In terms of consequences associated with the potential transfer of ARGs to human pathogens, we argue that unknown resistance genes are of greater concern than those already known to circulate among human-associated bacteria (6).
This study describes the potential for many external environments, including those subjected to pharmaceutical pollution, air and wastewater/sludge, to serve as hotspots for resistance development and/or transmission of ARGs. In addition, our results indicate that these environments may play important roles in the mobilization of yet unknown ARGs and their further transmission to human pathogens. To provide guidance for risk-reducing actions we – based on this study – suggest strict regulatory measures of waste discharges from pharmaceutical industries and encourage more attention to air in the transmission of antibiotic resistance (1).
References
- Pal C, Bengtsson-Palme J, Kristiansson E, Larsson DGJ: The structure and diversity of human, animal and environmental resistomes. Microbiome, 4, 54 (2016). doi: 10.1186/s40168-016-0199-5
- Durso LM, Miller DN, Wienhold BJ. Distribution and quantification of antibiotic resistant genes and bacteria across agricultural and non-agricultural metagenomes. PLoS One. 2012;7:e48325.
- Nesme J, Delmont TO, Monier J, Vogel TM. Large-scale metagenomic-based study of antibiotic resistance in the environment. Curr Biol. 2014;24:1096–100.
- Fitzpatrick D, Walsh F. Antibiotic resistance genes across a wide variety of metagenomes. FEMS Microbiol Ecol. 2016. doi:10.1093/femsec/fiv168.
- Allen HK, Moe LA, Rodbumrer J, Gaarder A, Handelsman J. Functional metagenomics reveals diverse β-lactamases in a remote Alaskan soil. ISME J. 2009;3:243–51.
- Bengtsson-Palme J, Larsson DGJ: Antibiotic resistance genes in the environment: prioritizing risks. Nature Reviews Microbiology, 13, 369 (2015). doi: 10.1038/nrmicro3399-c1
Published paper: Antibiotic resistance in sewage treatment plants
 After a long wait (1), Science of the Total Environment has finally decided to make our paper on selection of antibiotic resistance genes in sewage treatment plants (STPs) available (2). STPs are often suggested to be “hotspots” for emergence and dissemination of antibiotic-resistant bacteria (3-6). However, we actually do not know if the selection pressures within STPs, that can be caused either by residual antibiotics or other co-selective agents, are sufficiently large to specifically promote resistance. To better understand this, we used shotgun metagenomic sequencing of samples from different steps of the treatment process (incoming water, treated water, primary sludge, recirculated sludge and digested sludge) in three Swedish STPs in the Stockholm area to characterize the frequencies of resistance genes to antibiotics, biocides and metal, as well as mobile genetic elements and taxonomic composition. In parallel, we also measured concentrations of antibiotics, biocides and metals.
After a long wait (1), Science of the Total Environment has finally decided to make our paper on selection of antibiotic resistance genes in sewage treatment plants (STPs) available (2). STPs are often suggested to be “hotspots” for emergence and dissemination of antibiotic-resistant bacteria (3-6). However, we actually do not know if the selection pressures within STPs, that can be caused either by residual antibiotics or other co-selective agents, are sufficiently large to specifically promote resistance. To better understand this, we used shotgun metagenomic sequencing of samples from different steps of the treatment process (incoming water, treated water, primary sludge, recirculated sludge and digested sludge) in three Swedish STPs in the Stockholm area to characterize the frequencies of resistance genes to antibiotics, biocides and metal, as well as mobile genetic elements and taxonomic composition. In parallel, we also measured concentrations of antibiotics, biocides and metals.
We found that only the concentrations of tetracycline and ciprofloxacin in the influent water were above those that we predict to cause resistance selection (7). However, there was no consistent enrichment of resistance genes to any particular class of antibiotics in the STPs, neither for biocide and metal resistance genes. Instead, the most substantial change of the bacterial communities compared to human feces (sampled from Swedes in another study of ours (8)) occurred already in the sewage pipes, and was manifested by a strong shift from obligate to facultative anaerobes. Through the treatment process, resistance genes against antibiotics, biocides and metals were not reduced to the same extent as fecal bacteria were.
Worryingly, the OXA-48 beta-lactamase gene was consistently enriched in surplus and digested sludge. OXA-48 is still rare in Swedish clinical isolates (9), but provides resistance to carbapenems, one of our most critically important classes of antibiotics. However, taken together metagenomic sequencing did not provide clear support for any specific selection of antibiotic resistance. Rather, since stronger selective forces affect gross taxonomic composition, and thereby also resistance gene abundances, it is very hard to interpret the metagenomic data from a risk-for-selection perspective. We therefore think that comprehensive analyses of resistant vs. non-resistant strains within relevant species are warranted.
Taken together, the main take-home messages of the paper (2) are:
- There were no apparent evidence for direct selection of resistance genes by antibiotics or co-selection by biocides or metals
- Abiotic factors (mostly oxygen availability) strongly shape taxonomy and seems to be driving changes of resistance genes
- Metagenomic and/or PCR-based community studies may not be sufficiently sensitive to detect selection effects, as important shifts towards resistant may occur within species and not on the community level
- The concentrations of antibiotics, biocides and metals were overall reduced, but not removed in STPs. Incoming concentrations of antibiotics in Swedish STPs are generally low
- Resistance genes are overall reduced through the treatment process, but far from eliminated
References and notes
- Okay, those who takes notes know that I have already complained once before on Science of the Total Environment’s ridiculously long production handling times. But, seriously, how can a journal’s production team return the proofs for after three days of acceptance, and then wait seven weeks before putting the final proofs online? I still wonder what is going on beyond the scenes, which is totally obscure because the production office also refuses to respond to e-mails. Not a nice publishing experience this time either.
- Bengtsson-Palme J, Hammarén R, Pal C, Östman M, Björlenius B, Flach C-F, Kristiansson E, Fick J, Tysklind M, Larsson DGJ: Elucidating selection processes for antibiotic resistance in sewage treatment plants using metagenomics. Science of the Total Environment, in press (2016). doi: 10.1016/j.scitotenv.2016.06.228 [Paper link]
- Rizzo L, Manaia C, Merlin C, Schwartz T, Dagot C, Ploy MC, Michael I, Fatta-Kassinos D: Urban wastewater treatment plants as hotspots for antibiotic resistant bacteria and genes spread into the environment: a review. Science of the Total Environment, 447, 345–360 (2013). doi: 10.1016/j.scitotenv.2013.01.032
- Laht M, Karkman A, Voolaid V, Ritz C, Tenson T, Virta M, Kisand V: Abundances of Tetracycline, Sulphonamide and Beta-Lactam Antibiotic Resistance Genes in Conventional Wastewater Treatment Plants (WWTPs) with Different Waste Load. PLoS ONE, 9, e103705 (2014). doi: 10.1371/journal.pone.0103705
- Yang Y, Li B, Zou S, Fang HHP, Zhang T: Fate of antibiotic resistance genes in sewage treatment plant revealed by metagenomic approach. Water Research, 62, 97–106 (2014). doi: 10.1016/j.watres.2014.05.019
- Berendonk TU, Manaia CM, Merlin C, Fatta-Kassinos D, Cytryn E, Walsh F, et al.: Tackling antibiotic resistance: the environmental framework. Nature Reviews Microbiology, 13, 310–317 (2015). doi: 10.1038/nrmicro3439
- Bengtsson-Palme J, Larsson DGJ: Concentrations of antibiotics predicted to select for resistant bacteria: Proposed limits for environmental regulation. Environment International, 86, 140–149 (2016). doi: 10.1016/j.envint.2015.10.015
- Bengtsson-Palme J, Angelin M, Huss M, Kjellqvist S, Kristiansson E, Palmgren H, Larsson DGJ, Johansson A: The human gut microbiome as a transporter of antibiotic resistance genes between continents. Antimicrobial Agents and Chemotherapy, 59, 10, 6551–6560 (2015). doi: 10.1128/AAC.00933-15
- Hellman J, Aspevall O, Bengtsson B, Pringle M: SWEDRES-SVARM 2014. Consumption of antimicrobials and occurrence of antimicrobial resistance in Sweden. Public Health Agency of Sweden and National Veterinary Institute, Solna/Uppsala, Sweden. Report No.: 14027. Available from: http://www.folkhalsomyndigheten.se/publicerat-material/ (2014)